Home / Knowledge hub /
The pMDI dilemma: managing patient needs, human health, and the planet
April 7, 2023

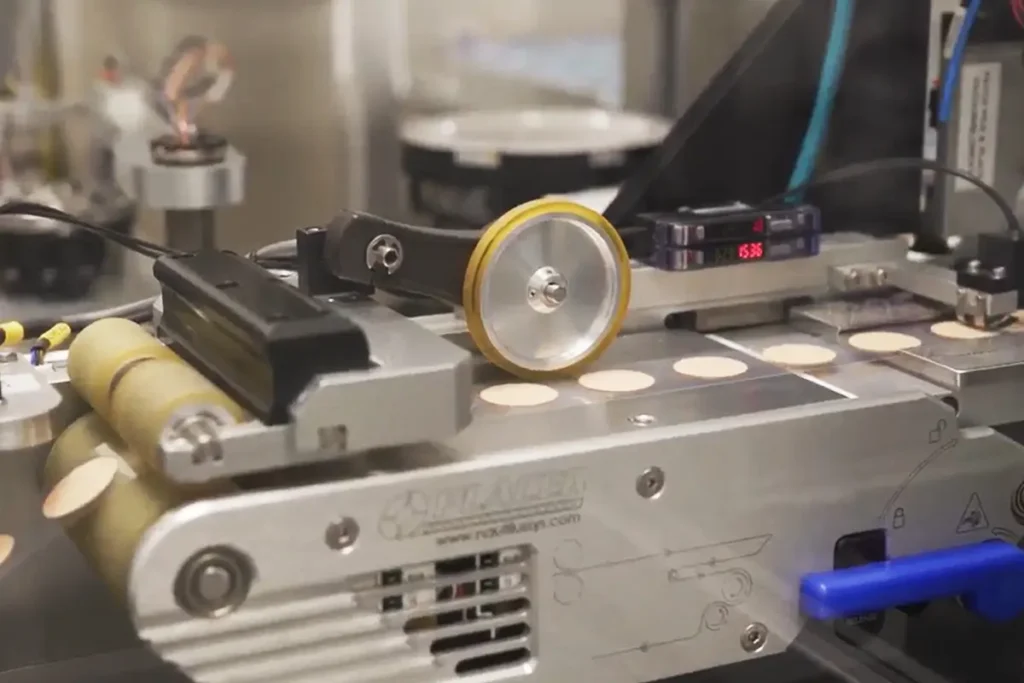
While long a topic of discussion, an even brighter spotlight has illuminated the subject of more environmentally friendly inhalers of late, thanks in part to the proposed phasedown on per- and polyfluoroalkyl substances (PFAS). PFAS substances as a class are comprised of thousands of synthetic chemicals that resist degradation because of their exceptionally strong chemical bonds, making them “forever” chemicals that may have an impact on human health and the environment. Due to their usefulness and consequent ubiquity, any regulatory shifts regarding their usage have the potential to impact a massive range of products across nearly every industry.
The European Chemicals Agency (ECHA) published a PFAS restriction proposal including ~10,000 substances on February 7, 2023, which is now under review by their scientific committees. Following the 6-month consultation period that began on March 22, 2023, the ECHA committees will share their opinions with the European Commission for evaluation and possible adoption.
This PFAS restriction proposal adds to concurrent legislation centered around reducing the use of fluorinated gases (F-gas). While the new regulations are aimed at curbing large-scale emissions from refrigeration and industrial usage, they would phase out compounds currently employed as propellants in many inhalers. These proposals have already accelerated shifts within the pharmaceutical sector, where consequences will be felt throughout the drug-device development pathway, including in manufacturing processes and supply chain reliability.
The Balancing Act
Having led the move from CFC to HFA propellants in the 1990s with the first CFC-free pressurized metered-dose inhaler (pMDI), we fully understand the challenges that arise from these kinds of transitions. Our experience has also cemented within our organization the importance of formulating and developing with all potential propellants, a proactive plan that should be part of every MDI company’s long-term strategy.
Some contemporary arguments offer a binary approach to the path ahead for inhalers, suggesting that switching to dry powder inhalers (DPIs) instead of pMDIs is the only answer, but the decision is more nuanced than that. While the transition to a more carbon neutral and sustainable industry is important, only by thoroughly evaluating (A) the implications to patients, (B) the broader picture of environmental waste, and (C) the full scope of available options can that goal be satisfied.
(A) The Patient
As with every transition in our industry, the welfare of patients is paramount, so although guidelines may shift to favor DPIs, it is vital that the appropriate path forward for each set of products respects the totality of patient needs. This includes the availability of products that are safe, effective, and usable, as well as the maintenance of a healthy environment. For example, some individuals are unable to generate adequate inspiratory flow to operate a DPI, immediately dispelling the idea that there is a single, one-size-fits-all solution that can satisfy the needs of both patients and the planet. Beyond this unambiguous instance, a tapestry of questions centered on patient welfare must also be addressed, including whether the patient is able to learn to use a new device correctly and whether the change will otherwise negatively impact adherence. The pharmaceutical industry exists to improve the lives of those in need, so these decisions must always be made on the basis of what is best for the overall health of the patient.
(B) The Planet
Our understanding of the industry’s environmental effects must constantly expand, and adaptations to improve them must be ongoing. While the development of green propellants is an important factor, the evaluation must incorporate the damage caused by chemical components alongside that caused by all other factors, including component materials and how recyclable they are. For example, while much of the current focus is on propellants used in pMDIs, an evaluation of the depletion of fossil resources by the University of Manchester, U.K., found DPIs to have the most damaging impact. Taking a wider viewpoint helps provide a more complete understanding of problem areas from creation to use and disposal, allowing a full accounting of the carbon footprint for each therapy. In order to provide effective medicines that do as little harm to the planet as possible, it is imperative to move away from siloed thinking and toward holistic solutions.
(C) The Possibilities
To realize a future that satisfies patient needs while also meeting those of the planet and general human health, innovation must be realized across the gamut of effective therapies and devices. Notable exceptions aside, discovery often happens when people are searching. If lines of treatment are abandoned entirely, there is a grave risk of losing consequential innovations — if not in the therapy or device itself, then in an undiscovered manufacturing method or shipping advancement. Every avenue of improvement begets more opportunities for something transformational to be uncovered. In the current environment for MDIs, this means continuous research and development of green propellants, such as HFC-152a (which is itself a good, but not universal, alternative) for commercial use, as well as HFO-1234ze, which could be restricted through PFAS regulations despite having a 99.9% lower Global Warming Potential (GWP) than P134a, the greenest option in use today.
This ongoing exploration of solutions represents one of the things the industry as a whole does best: find new ways forward in the face of emerging difficulties. Even with the unexpected hurdles common to drug and device development, it can be easy to forget that ideal solutions rarely continue their run with that title intact. As with our transition from CFCs to HFAs decades ago, when the industry must grapple with new challenges, novel optimal solutions are needed. Ongoing development across multiple therapies, products, and delivery methods ensures patients have an acceptable alternative whenever a newly discovered adjustment needs to be made to an existing therapy.
Propagating Progress
With all of this in mind, what can you do to prepare your combination drug-device product to optimally serve the holistic needs of patients and our planet?
- Stay up to speed on current regulations and what is coming down the pipeline. Guiding from the trends you see developing, create an informed strategy that anticipates future issues.
- Know the full footprint of your product. Identifying all the ways you can optimize your processes now can give you a head start when new regulations arise.
- Choose an experienced partner with a demonstrated history of adaptability and innovation. Between their institutional knowledge and hands-on know-how, the right CDMO can help you quickly identify the best path forward and get you there.
- Find the right capabilities for switching faster than your competitors, which means making sure to explore how far along your CDMO is in upgrading to green propellants. Additionally, look for a partner who can provide manufacturing services with a variety of propellants, so you are covered no matter what legislation comes next.
As ECHA, the European Commission, and the entire drug-device industry take a long hard look at what propellants and materials are safe for the planet, it can be easy to miss the larger picture and even lose patients in the conversation altogether. Given that inhalers and similar medical devices exist specifically to assist them, it is vital that patients are central to the conversation. Meeting their therapeutic needs while protecting the planet as a whole, however, requires a wide-lens view.
The most ideal therapy for the patient is the one that is safe, effective, affordable, and promotes easy adherence, and at times, that will not be the greenest therapy. But it could likely be greener. Evaluating the full footprint of every therapy allows the industry to truly address its environmental impact and meet every patient’s needs with a more environmentally sound treatment. This big-picture approach puts patients at the forefront while proactively moving the industry on the path to a more sustainable future. To continually improve therapies while safeguarding the array of options that best meet tailored patient treatment plans, the search for greener solutions must be developed with the holistic well-being of patients now and in the future top of mind.
Explore how Kindeva Drug Delivery is leading the industry in bringing green propellants to commercial drug-device manufacturing.
Related resources
Explore our other resources to discover valuable insights on the latest trends in drug delivery.
Career journeys blog 4: Grace Guo
In this story, we meet Grace Guo, Manager of Client Portfolio Relationship Management, whose pathway at Kindeva has grown through clear communication, strategic thinking and a strong focus on people.
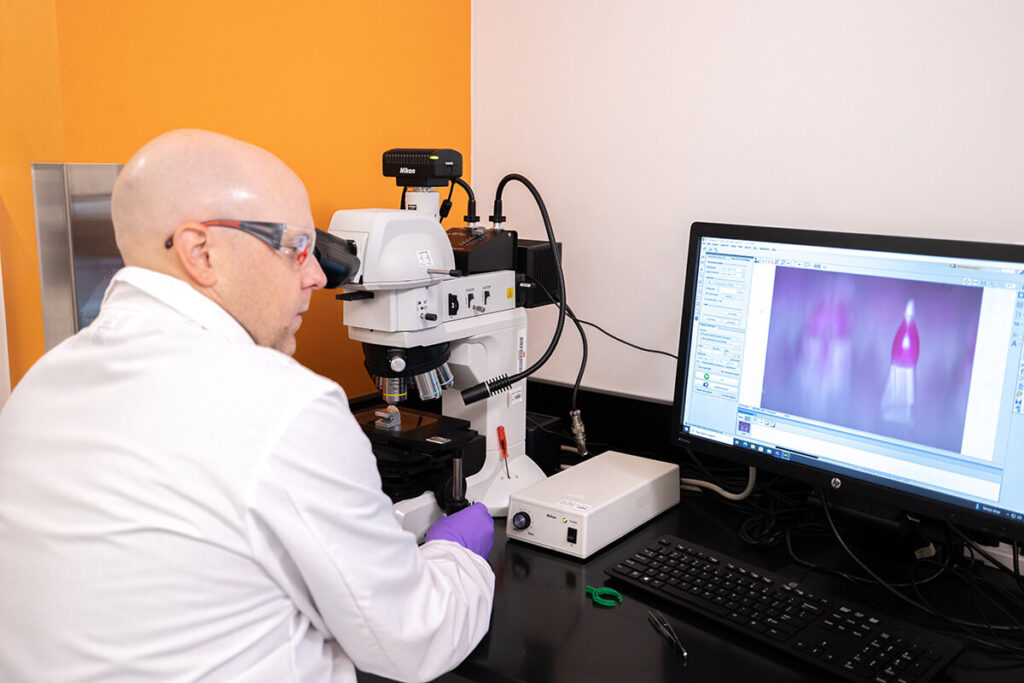
Learn MoreThe next leap in skin-based drug delivery: How dermal delivery platforms are transforming tomorrows for patients
Skin-based drug delivery is gaining attention as patients and healthcare systems look for treatments that support at-home administration and remove the need for needle-based injections. As this shift accelerates, developers are investing in technologies that improve usability without compromising performance. These platforms are opening new possibilities for therapies that rely on reliable, patient-preferred delivery. A […]
Learn MoreWebinar | A Bridge to the Future of Aseptic Manufacturing: A Pharma 4.0 Case Study
Growing demand for high-quality sterile fill finish capacity is putting pressure on development timelines and supply programs across the industry. As expectations for Annex 1 alignment, agility and data-driven control rise, partners need facilities designed to keep pace with evolving requirements. In this on-demand webinar, Chad Hafer, Director of Technical Operations, Aseptic Fill Finish at […]
Learn MoreCareer journeys blog 3: Lauren Harrison
In this story, we meet Lauren Harrison, a formulation scientist who began her path as an apprentice and has spent the last decade building a career rooted in curiosity, hands-on learning and collaboration.
Learn MoreNavigating the transition to next-generation propellants for pMDIs | On-demand webinar
Regulators, health systems and patients expect meaningful progress on sustainability. For pressurized metered dose inhalers (pMDIs), this means planning the transition to low global warming potential (low-GWP) next-generation propellants (NGPs) now, not at the end of the decade. In this webinar with Pharmaceutical Technology, Craig Somerville, Senior Vice President of Kindeva’s pMDI business unit, shares […]
Learn MoreBeyond the contract: Driving transformational partnerships with manufacturing… and more
Achieving scientific breakthroughs is just one hurdle in today’s drug development and manufacturing process aimed at improving patient outcomes. Bringing a new therapy to market requires meticulous execution and clear communication at every step. Unfortunately, even the most groundbreaking scientific advancements can be delayed or even entirely abandoned due to poor performance from partners. This […]
Learn MoreWhy Kindeva: Analytical and regulatory services
Overcome complex analytical and regulatory challenges with a partner dedicated to your product’s success. Our specialist expertise helps you navigate testing, compliance, and quality to advance your project from concept to commercialization. Download our one-pager for a closer look at our integrated approach, including: An overview of our comprehensive, phase-appropriate analytical services. How our regulatory […]
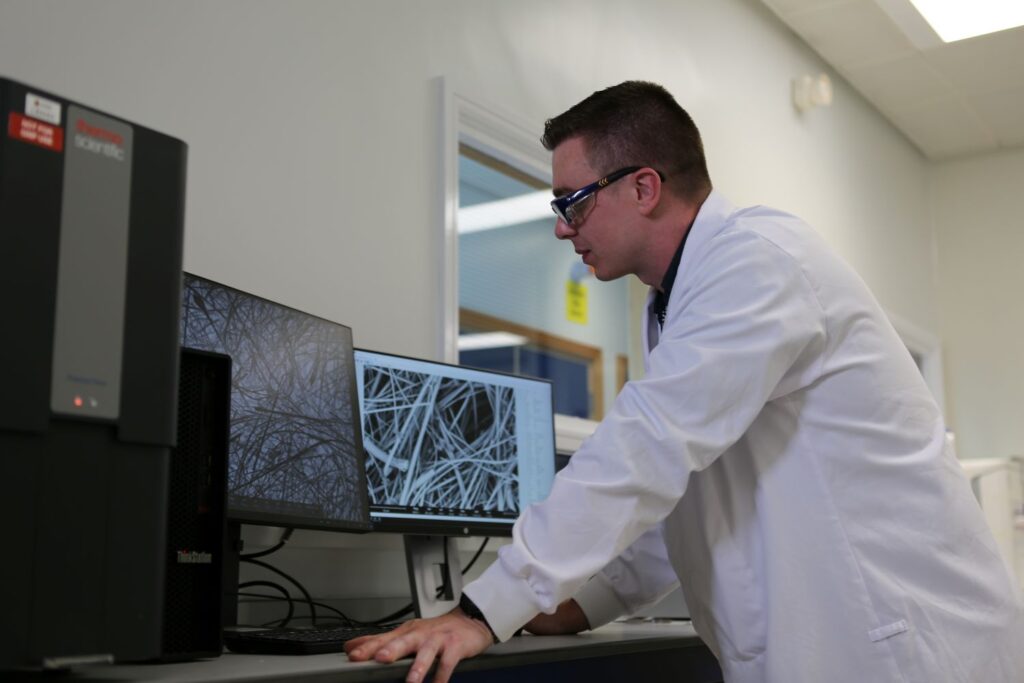
Learn MoreCareer journeys blog 2: Oliver Ingham
In this latest installment, we meet Oliver Ingham, an analytical chemist whose curiosity and problem-solving skills have shaped his journey from academic research to coordinating analytical development services at Kindeva.
Learn MoreCareer journeys blog 1: Holly Dowdle
When Holly Dowdle first joined Kindeva as a student intern, she experienced a workplace that valued both curiosity and collaboration. It was an environment where asking questions was encouraged and development was part of everyday work, not something that happened on the sidelines.
Learn MoreLet’s transform tomorrow together
Every patient deserves a brighter tomorrow. As your strategic partner, we are dedicated to building your lasting legacy and helping you fast-track healthier tomorrows. You dream it, we deliver it.